Understanding the relationship between viral persistence and the incidence of symptom recurrence in Ebola virus disease survivors
Abstracts
Scientific Abstract
Ebolavirus is a lethal pathogen that causes hemorrhagic fever following direct contact with contaminated body fluids and is responsible for several outbreaks over the last forty years. The possibility for viral persistence to occur following recovery from infection has been documented during recent outbreaks, but the consequences of that persistence still remain unknown. The objective of this study is to determine the role that viral persistence plays in the recurrence of Ebola virus disease symptoms. Utilizing a prospective cohort design, survivors of the 2020 outbreak in Equateur Province of the Democratic Republic of the Congo will be tested for viral persistence at regular intervals and surveyed to identify incidents of symptom recurrence over a two-year period. Initial testing will determine a baseline of participants’ health and viral status post-infection. Subsequent testing of blood and semen at three-month intervals will determine the prevalence of viral persistence in the cohort. Responses to questionnaires completed during sampling will provide information on symptom recurrence and immune competency during the study period. The results of this study should provide valuable information on the frequency of viral persistence, the prevalence of symptom recurrence and the risk of recurrence associated with persistence. These findings will allow survivors and healthcare workers to take appropriate precautions following recovery from infection.
Public Abstract
Ebolavirus has caused multiple outbreaks of hemorrhagic fever in recent years. Survivors of infection have been found to harbor the virus well after they have recovered, but we are still learning what impacts that has on the patient and the community. This study looks at the association between viral persistence after infection and the recurrence of Ebola virus disease (EVD) symptoms in survivors of the most recent outbreak. Participants will be tested at regular intervals and monitored for symptoms of EVD. This study will provide a greater understanding of the continued risks to EVD survivors after recovery.
Introduction
Ebola virus disease (EVD) is still a relatively new infectious disease, with the first outbreaks occurring in 1976 in Sub-Saharan Africa (1). EVD is caused by one of four species of Ebolavirus: Zaire ebolavirus, Sudan ebolavirus, Taï Forest ebolavirus (previously Côte d’Ivoire ebolavirus), and Bundibugyo ebolavirus (1). Two additional species of Ebolavirus, Reston ebolavirus and Bombali ebolavirus, have not been found to cause disease in humans (1). These viruses are members of the Filoviridae family which are characterized by long, filamentous viral particles (2). They are enveloped viruses composed of negative-sense, single-stranded RNA (2).
The first case of Ebola virus disease occurred in what is now the Democratic Republic of the Congo, near the Ebola River (2). Initially misdiagnosed with malaria, the patient was treated at a local hospital where a lack of good hygiene practices facilitated spread of the virus among other patients (2). Of the more than 300 people infected during this outbreak, nearly 90% died from the disease (2). A second outbreak took place in nearby Sudan that same year that was thought to be linked to the first (2). Subsequent study of the causative agent has shown that these outbreaks were caused by two distinct species of Ebolavirus, Zaire ebolavirus and Sudan ebolavirus, and sporadic outbreaks have occurred throughout Africa since 1976 (2).
Transmission of Ebolavirus occurs through direct contact with contaminated blood, body fluids, or surfaces containing the virus (1). It is believed to have an infectious dose of less than 10 viral particles, making proper sanitation critical to preventing spread of the disease (2). The limited resources of field hospitals in Sub-Saharan Africa increases the risk of transmission to both medical personnel and patients (2). The virus can incubate within the body for up to 21 days before causing symptoms (1). Prior to the appearance of symptoms, the viral load is thought to be too low for transmission (2). Fruit bats are believed to be the natural reservoirs for the virus and infection occurs through direct contact with infected body fluids or meat of bats or other infected animals (2).
Once infected, Ebola virus disease begins with nonspecific viral symptoms that include fever, myalgia, fatigue, weakness, and headaches (4). Some patients also develop nausea and diarrhea (4). The disease may then progress to unexplained bleeding throughout the body including from the gums, nose, eyes, skin, and gastrointestinal tract (4). The final stage of EVD is hemorrhagic fever which is characterized by damage to blood vessels that causes uncontrollable internal and external bleeding leading to death (2, 4). The mortality rate varies from 25 to 90% depending on the species of Ebolavirus involved (2).
Until recently, there has been no specific treatment for EVD outside of supportive care that includes blood and fluid replacement, pain and fever management, oxygen therapy and antiemetics (4). Secondary bacterial infections were treated with antibiotic therapy as they occurred (4). The lack of treatment options meant that survival of the disease depended on the virulence of the virus and the individual’s immune system (2). In recent outbreaks, the World Health Organization provisionally approved the use of four investigational drugs to help in the treatment of patients. Regeneron (REGN-EB3) and mAb114, monoclonal antibodies for treatment of Zaire ebolavirus, were shown to improve the survival rates of EVD patients (4, 17).
During the 2015 outbreak, an experimental vaccine for Zaire ebolavirus was tested to help prevent transmission of the disease in Guinea (3) and the results of this trial showed the vaccine, rVSV-ZEBOV, to be highly effective (4).The vaccine was deployed in a ring vaccination strategy during the 2018 outbreak in the DRC and found to be over 90% effective in preventing or reducing the severity of illness (5). The vaccine has since been approved by European regulators, prequalified by the WHO (6), and approved by the United States Food and Drug Administration (3).
Literature Review
Knowing the true number of cases of Ebolavirus infection is a key component of understanding the virus. Along with known cases, measuring the seropositivity rate in areas where outbreaks have occurred can provide additional measure of incidence (9, 10). A 1997 survey of 8 villages in Gabon, which had experienced several outbreaks, revealed a low rate of seropositivity among those without a history of Ebolavirus infection (9). During the 2014 outbreak in Sierra Leone, a late phase population-based study founds high rates of seropositivity among confirmed cases (10). This would indicate that the presences of antibodies in patients indicates prior infection, with seropositivity being used to study the prevalence of asymptomatic cases (8).
A primary focus during outbreaks has been to reduce the mortality rate. Historically, these efforts have been taken through case detection and treatment of symptoms. Recent technological advances have produced therapeutics with the goal of improving the survival rate. During the 2014 outbreak, a randomized control trial utilizing ZMapp, a monoclonal antibody treatment, suggested a 40% reduction in the relative risk of mortality in confirmed cases (16). A subsequent trial during the 2018 outbreak found it to be less effective than two other newly developed therapies, MAb114 and REGN-EB3, which reduced the risk of mortality by 14.6% and 17.8% respectively compared to ZMapp (17). The initial ZMapp study was hampered by the ending of the outbreak and a reduction in available cases (16), but was used during the initial stages of the 2018 outbreak until more effective treatments were found (17).
While the ZMapp study did not see a predictive relationship between viral load and outcomes (16), the subsequent study of treatments did find statistical evidence that a high viral load correlated with a greater risk of death (17). This finding has been supported by multiple studies that looked for predictors of survival in Ebola patients (12-14). Retrospective cohort studies found that age and viral load correlated with mortality (13), and that viral load at admission correlated with mortality (14).
A retrospective cohort study found that the extent of organ damage in all Ebola virus disease patients was associated with the viral load (15). The importance of viral load in mortality was further emphasized by a separate retrospective cohort study, but was not found to correlate with sequelae in survivors (12). The incidence and persistence of post-viral symptoms was studied in a longitudinal case control study, and found to resolve over time with indications based on the control population that symptoms may be unrelated to Ebolavirus infection (11). The conflicting results of these studies showing the association of viral load with organ damage but not predictive of sequelae should be further explored.
The longitudinal case control study also looked at viral persistence in recovered cases and found the virus could be detected in semen for up to forty months after infection, which could lead to clusters of cases after active transmission within a population has ended (11). The persistence, and potential recurrence, of Ebolavirus following recovery was investigated during a case study of a familial cluster in Sierra Leone in 2015 (7). While the individual believed to be responsible for transmitting the virus was never a confirmed case, the high levels of antibodies were indicative of past infection (7, 10). The study began after a child was diagnosed with EVD despite no traceable contacts with active infections, and concluded the likely transmission was child’s mother who had been treated for illness following childbirth (7). The medical history for the mother led researchers to conclude that she had initially been infected with Ebolavirus during the active outbreak over one year earlier and the stress of a recent childbirth resulted in a recurrence of symptoms and transmission to her child and husband (7).
Proposal
Despite four decades having passed since the first known case of Ebola virus disease, there are still many unknown factors about the virus and the disease it causes (7, 8). Ebolavirus has been known historically for its ability to cause death (2). It is only from studies related to recent outbreaks that we’ve learned more about the virus, how to contain it, and how to treat it (2). This includes more information on the prevalence of asymptomatic cases and the ability for the virus to persist in some body fluids well beyond recovery (8). As noted by a case study on recurrence of EVD, an area that needs further investigation is viral persistence and its consequences (7).
Individual cases studies have been conducted on patients who demonstrate a recurrence of symptoms (7); however, a widespread study has yet to be conducted among EVD survivors. A longitudinal case-control study found that viral persistence can contribute to increased risk of sequelae (11). Additionally, the prolonged testing of semen conducted during the study revealed that Ebolavirus may persist in body fluids at varying levels for much longer than previously believed (11). One question that still needs to be answered is: does viral persistence increase the incidence of symptom recurrence in EVD survivors?
Based on the work of case-control study, it appears there is an association between these factors that should be further investigated (11). If the recurrence of symptoms in Ebola virus disease survivors is related to viral persistence after recovery, then survivors with detectable levels of the virus will have an increased rate of symptom recurrence.This prospective cohort study aims to follow at least one hundred EVD survivors in Equateur Province of the Democratic Republic of the Congo (DRC) from the ongoing 2020 outbreak, confirmed either by a positive RT-PCR blood test during infection or a positive IgG blood test following recovery.
Participants will be tested at intervals for viral persistence in blood and semen. The testing of semen has been chosen due to existing data indicating Ebolavirus has greater persistence in sites that are immune privileged (7). Testing of fluids from other immune privileged sites would be invasive and present additional risks to participants, such as spinal taps to obtain cerebrospinal fluid. Initial testing for viral persistence will be conducted within one month of recovery from symptoms or medical discharge. This will include an RT-PCR test, IgG test, IgM test and a survey to ascertain a health baseline following the initial infection. Subsequent testing of blood and semen, along with follow up surveying will be conducted every 3 months for a period totaling 2 years. This is due to the potential for intermittent shedding of the virus which could impact regular detection (11). During these tests, participants will also be asked to complete a survey regarding recent symptoms and conditions including any illness or unusual stress events. Relevant stress events include onset of new, unrelated conditions that may weaken their immune system, such as cancer, diabetes, or cardiopulmonary disease.
Participants must be adult males, aged 18 to 65 years old, located in the Equateur Province of the DRC, have a recent history of EVD related to the 2020 outbreak, and otherwise be in good health. Potential candidates will be recruited based on either medical history of an EVD diagnosis or self-reported illness fitting the case definition. Participants who do not have a history of a positive RT-PCR blood test for Ebolavirus will only be included if they test positive for Ebolavirus-specific IgG antibodies at the onset of the study. This study will exclude children under the age of 18 for ethical reasons. Those with underlying chronic health conditions that cause recurrent illness or impact their immune competency will be excluded to avoid conflating the pre-existing disease and recurrence. Anyone who has received a vaccine against Ebolavirus would also be excluded from the study.
The World Health Organization’s case definition will be used to determine potential recurrence events. Cases of recurrence would include any participant reporting sudden onset of fever and at least three of the following symptoms: headaches, loss of appetite, stomach pain, vomiting, diarrhea, lethargy, myalgia, arthralgia, difficulty swallowing, difficulty breathing or hiccups (18). Any participants who experience inexplicable bleeding regardless of fever or other symptoms would be identified as having a recurrence of symptoms (18). The sudden death of any participant that cannot be explained by other causes would also be identified as a recurrence (18). Those reporting active or recent symptoms fitting this case definition will undergo additional testing including IgM levels that would indicate an active or recent infection (7). Contact tracing for all participants reporting a recurrence of symptoms will be completed to rule out a secondary exposure.
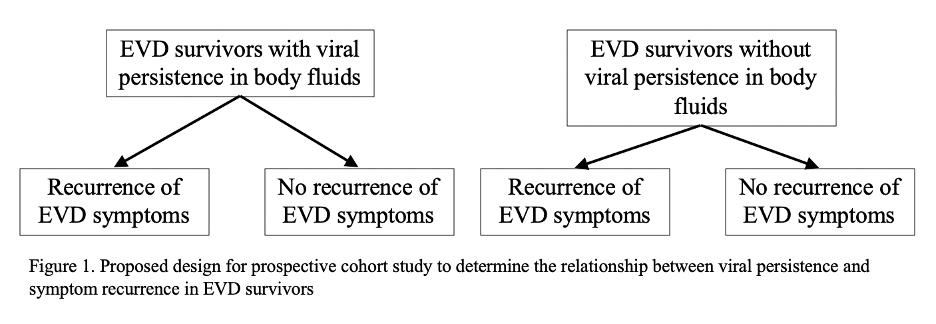
For this study, the risk factor for symptom recurrence is viral persistence. Initial findings from related studies indicate that immune suppressing events may increase the chances of recurrence (7). Participants will be asked about these events during the course of the study to aid in data analysis, but occurrence does not change the study protocol. Data will be broken down based on the study design once all testing has been completed. The two groups will consist of those with viral persistence detected at 3 months or more from the initial recovery and those without viral persistence detected. Each group will then be analyzed for incidents of recurrence and compared based on demographics including age, sex, economic status, health over the course of the study, and treatment received for the initial infection.
Computational analysis of the prevalence of recurrence and the relative risk related to viral persistence will be used to draw conclusions. The incidence of symptom recurrence in both the group with detectable viral persistence and without is calculated based on the number of survivors that experience symptom recurrence out of the total number of survivors within the group (19). Relative risk is determined based on the incidence of EVD symptom recurrence in survivors with detectable viral persistence compared to the incidence of symptom recurrence in survivors without detectable viral persistence (19). A relative risk greater than 1.0 would indicate that viral persistence increases the risk for symptom recurrence (19). If the relative risk is 1.0 or less then viral persistence is not likely to be related to the risk of symptom recurrence and the data should be reviewed for other potential sources of risk (19).
The complete timeline for this study will depend, in large part, on the ability to enroll participants. The progression of the outbreak is difficult to predict and will impact the ability to enroll survivors. Close contact tracing of known cases and antibody testing of those reporting EVD-like symptoms can be used to aid recruitment. If enough participants can be enrolled within 6 months, then the collection of data will be completed by two and a half years from when the study began. Allowing time for full data analysis, results could be seen within three years.
References
1. CDC. 2019. Ebola (Ebola Virus Disease): What is Ebola virus disease? https://www.cdc.gov/vhf/ebola/about.html. Accessed
2. Medicine BCo. Ebola Virus. https://www.bcm.edu/departments/molecular-virology-and-microbiology/emerging-infections-and-biodefense/ebola-virus. Accessed
3. CDC. 2019. Ebola (Ebola Virus Disease): Prevention and Vaccine. https://www.cdc.gov/vhf/ebola/prevention/index.html. Accessed
4. WHO. 2020. Ebola virus disease. https://www.who.int/en/news-room/fact-sheets/detail/ebola-virus-disease. Accessed
5. WHO. 2019. Preliminary results on the efficacy of rVSV-ZEBOV-GP Ebola vaccine using the ring vaccination strategy in the control of an Ebola outbreak in the Democratic Republic of the Congo: An example of integration of research into epidemic response. https://www.who.int/csr/resources/publications/ebola/ebola-ring-vaccination-results-12-april-2019.pdf?ua=1. Accessed
6. Callaway E. 2019. “Make Ebola a thing of the past:” First vaccine against the deadly virus approved. Nature 575:425-426.
7. Dokubo EK, Wendland A, Mate SE, Ladner JT, Hamblion EL, Raftery P, Blackley DJ, Laney AS, Mahmoud N, Wayne-Davies G, Hensley L, Stavale E, Fakoli L, Gregory C, Chen TH, Koryon A, Roth Allen D, Mann J, Hickey A, Saindon J, Badini M, Baller A, Clement P, Bolay F, Wapoe Y, Wiley MR, Logue J, Dighero-Kemp B, Higgs E, Gasasira A, Williams DE, Dahn B, Kateh F, Nyenswah T, Palacios G, Fallah MP. 2018. Persistence of Ebola virus after the end of widespread transmission in Liberia: an outbreak report. Lancet Infect Dis 18:1015-1024.
8. Diallo MSK, Rabilloud M, Ayouba A, Touré A, Thaurignac G, Keita AK, Butel C, Kpamou C, Barry TA, Sall MD, Camara I, Leroy S, Msellati P, Ecochard R, Peeters M, Sow MS, Delaporte E, Etard JF. 2019. Prevalence of infection among asymptomatic and paucisymptomatic contact persons exposed to Ebola virus in Guinea: a retrospective, cross-sectional observational study. Lancet Infect Dis 19:308-316.
9. Heffernan RT, Pambo B, Hatchett RJ, Leman PA, Swanepoel R, Ryder RW. 2005. Low Seroprevalence of IgG Antibodies to Ebola Virus in an Epidemic Zone: Ogooué-Ivindo Region, Northeastern Gabon, 1997. The Journal of Infectious Diseases 191:964-968.
10. Liu Y, Sun Y, Wu W, Li A, Yang X, Zhang S, Li C, Su Q, Cai S, Sun D, Hu H, Zhang Z, Yang X, Kamara I, Koroma S, Bangura G, Tia A, Kamara A, Lebby M, Kargbo B, Li J, Wang S, Dong X, Shu Y, Xu W, Gao GF, Wu G, Li D, Liu WJ, Liang M. 2018. Serological Investigation of Laboratory-Confirmed and Suspected Ebola Virus Disease Patients During the Late Phase of the Ebola Outbreak in Sierra Leone. Virol Sin 33:323-334.
11. Sneller MC, Reilly C, Badio M, Bishop RJ, Eghrari AO, Moses SJ, Johnson KL, Gayedyu-Dennis D, Hensley LE, Higgs ES, Nath A, Tuznik K, Varughese J, Jensen KS, Dighero-Kemp B, Neaton JD, Lane HC, Fallah MP.2019. A Longitudinal Study of Ebola Sequelae in Liberia. N Engl J Med 380:924-934.
12. Wing K, Oza S, Houlihan C, Glynn JR, Irvine S, Warrell CE, Simpson AJH, Boufkhed S, Sesay A, Vandi L, Sebba SC, Shetty P, Cummings R, Checchi F, McGowan CR. 2018. Surviving Ebola: A historical cohort study of Ebola mortality and survival in Sierra Leone 2014-2015. PLoS One 13:e0209655.
13. Li J, Duan HJ, Chen HY, Ji YJ, Zhang X, Rong YH, Xu Z, Sun LJ, Zhang JY, Liu LM, Jin B, Zhang J, Du N, Su HB, Teng GJ, Yuan Y, Qin EQ, Jia HJ, Wang S, Guo TS, Wang Y, Mu JS, Yan T, Li ZW, Dong Z, Nie WM, Jiang TJ, Li C, Gao XD, Ji D, Zhuang YJ, Li L, Wang LF, Li WG, Duan XZ, Lu YY, Sun ZQ, Kanu ABJ, Koroma SM, Zhao M, Ji JS, Wang FS. 2016. Age and Ebola viral load correlate with mortality and survival time in 288 Ebola virus disease patients. Int J Infect Dis 42:34-39.
14. Fitzpatrick G, Vogt F, Moi Gbabai OB, Decroo T, Keane M, De Clerck H, Grolla A, Brechard R, Stinson K, Van Herp M. 2015. The Contribution of Ebola Viral Load at Admission and Other Patient Characteristics to Mortality in a Médecins Sans Frontières Ebola Case Management Centre, Kailahun, Sierra Leone, June-October 2014. J Infect Dis 212:1752-8.
15. Lanini S, Portella G, Vairo F, Kobinger GP, Pesenti A, Langer M, Kabia S, Brogiato G, Amone J, Castilletti C, Miccio R, Capobianchi MR, Strada G, Zumla A, Di Caro A, Ippolito G. 2018. Relationship Between Viremia and Specific Organ Damage in Ebola Patients: A Cohort Study. Clin Infect Dis 66:36-44.
16. Davey RT, Jr., Dodd L, Proschan MA, Neaton J, Neuhaus Nordwall J, Koopmeiners JS, Beigel J, Tierney J, Lane HC, Fauci AS, Massaquoi MBF, Sahr F, Malvy D. 2016. A Randomized, Controlled Trial of ZMapp for Ebola Virus Infection. N Engl J Med 375:1448-1456.
17. Mulangu S, Dodd LE, Davey RT, Jr., Tshiani Mbaya O, Proschan M, Mukadi D, Lusakibanza Manzo M, Nzolo D, Tshomba Oloma A, Ibanda A, Ali R, Coulibaly S, Levine AC, Grais R, Diaz J, Lane HC, Muyembe-Tamfum JJ, Sivahera B, Camara M, Kojan R, Walker R, Dighero-Kemp B, Cao H, Mukumbayi P, Mbala-Kingebeni P, Ahuka S, Albert S, Bonnett T, Crozier I, Duvenhage M, Proffitt C, Teitelbaum M, Moench T, Aboulhab J, Barrett K, Cahill K, Cone K, Eckes R, Hensley L, Herpin B, Higgs E, Ledgerwood J, Pierson J, Smolskis M, Sow Y, Tierney J, Sivapalasingam S, Holman W, Gettinger N, Vallée D, et al. 2019. A Randomized, Controlled Trial of Ebola Virus Disease Therapeutics. N Engl J Med 381:2293-2303.
18. WHO. 2014. Case definition recommendations for Ebola or Marburg virus disease.
19. Ranganathan P, Aggarwal R, Pramesh CS. 2015. Common pitfalls in statistical analysis: Odds versus risk. Perspectives in clinical research 6:222-224.